It’s been a year since the first case of COVID-19 was identified in Wuhan, China, and in that time, we’ve gone from not even having a name for the disease to developing treatments and approving two vaccines for emergency use. Despite how far we’ve come, scientists are still hard at work finding more effective ways to treat for the disease. Many treatments being tested are already used for other diseases — in fact, you may even have heard of them before.
Here are four surprisingly ubiquitous drugs that are being tested as treatments for COVID-19.
The BCG Vaccine
Although you may not have heard of this vaccine, it’s one of the most widely used in the world, as well as one of the oldest. The Bacille Calmette-Guérin vaccine, named for the two French scientists who developed it, is one of the only vaccines being tested for COVID-19 that was created to prevent a completely different disease: tuberculosis (TB). It was developed a century ago in 1921, and is typically given outside the United States in areas where TB is still common. It’s also given to children in the U.S. who might be at particular risk for developing TB.
Unfortunately, the BCG vaccine is not consistently effective at preventing lung disease from TB, particularly in adults. But early on, researchers noticed that it seemed to reduce deaths from diseases that had nothing to do with TB. Since then, researchers have found that the vaccine has a wide range of beneficial effects on the immune system unrelated to TB, called off-target effects. A form of the vaccine is even approved in the U.S. as an immune therapy for patients with bladder cancer because of these unexpected benefits.
The vaccine has also shown some promise in treating respiratory infections like COVID-19, and studies examining the vaccine’s effect on COVID-19 have had some encouraging results. A study published in November showed that in a group of about 6,000 healthcare workers, those who had received the BCG vaccine previously were less likely to have had COVID-19 and generally had fewer symptoms.
“It would be wonderful if one of the oldest vaccines that we have could help defeat the world’s newest pandemic.”
“It would be wonderful if one of the oldest vaccines that we have could help defeat the world’s newest pandemic,” Dr. Moshe Arditi, director of the Pediatric and Infectious Diseases and Immunology Division at Cedars-Sinai Medical Center in Los Angeles and co-senior author of the study, said in a press release.
But an October analysis did not find a notable link between areas where the BCG vaccine is more frequently given and fewer deaths from COVID-19, despite earlier analyses that did. The World Health Organization also says there’s not yet enough evidence to say if the vaccine is useful against COVID-19.
Importantly, no true clinical trials, which compare those who receive the vaccine to people who get a placebo, have been completed. But there are more than two dozen current clinical trials of the vaccine related to COVID-19 worldwide, with one, a Mexican trial of 900 healthcare workers, due to be completed in January 2021. Although that trial and others might provide valuable data about how well the vaccine works against COVID-19, the first U.S. BCG trials aren’t set to finish until November 2021. Although the U.S. and other counties have already approved COVID-19-specific vaccines, the BCG vaccine, if proven effective against COVID-19, could still provide protection to people unable to get one of the new vaccines. “It is a potentially important bridge that could offer some benefit until we have the most effective and safe COVID-19 vaccines made widely available,” said Arditi. So a century-old TB vaccine could still become a valuable tool in fighting the COVID-19 pandemic.
Thalidomide
To many, the name of the drug thalidomide conjures up horrifying images of the public health crisis it once caused. In the later ’50s and early ’60s, many pregnant women took thalidomide to treat morning sickness. But the drug, which hadn’t been tested in pregnant women, caused severe birth defects, like stunted or missing limbs. The crisis was so severe that it prompted the U.S. to impose many of the strict guidelines for drug testing that we have today.

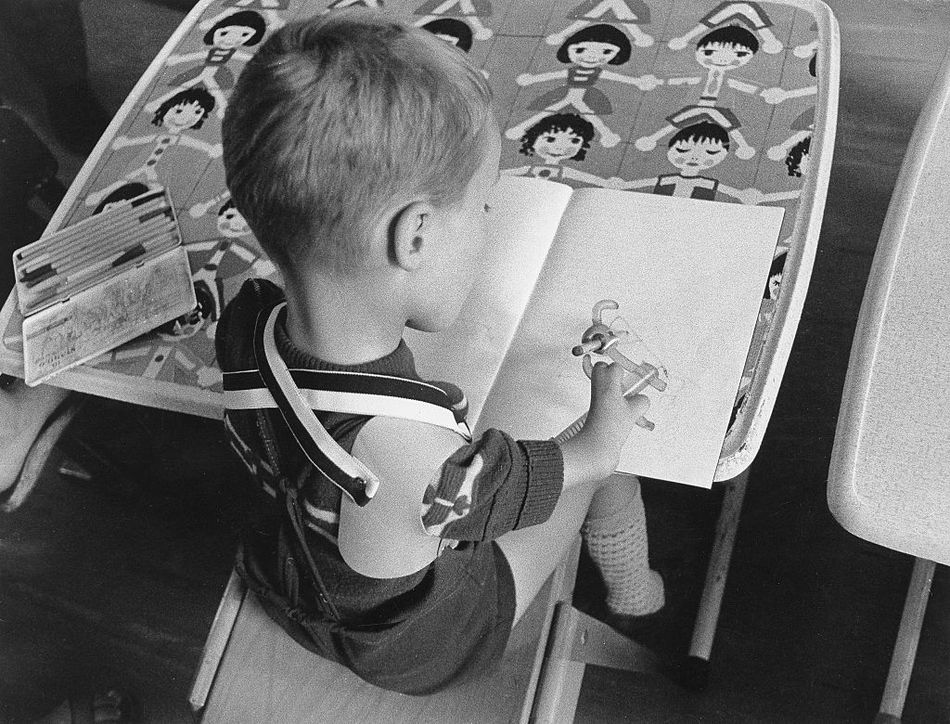
Children affected by thalidomide, like this boy, often had shortened, misshapen, or missing limbs.
Image: ullstein bild via Getty Images
Thalidomide is still used, although not for morning sickness. In the U.S., it’s approved to treat multiple myeloma, a type of blood cancer, and complications of leprosy. It’s also been investigated as a treatment for many other conditions, like the H1N1 “swine flu” and idiopathic pulmonary fibrosis, a chronic lung disease that causes scar tissue to grow in the lungs. A small 2012 study of 23 patients with this condition found that thalidomide improved cough and other respiratory symptoms.
Because thalidomide seems to decrease inflammation, can calm the immune system, and has had some success treating serious respiratory disease, some scientists think it could help decrease the inflammation that COVID-19 causes and combat a “cytokine storm” — an immune system overreaction that severe COVID-19 often induces.
So far, there’s very limited information on how well the drug might work as a treatment for COVID-19. A recent Chinese study retrospectively examined the effect of thalidomide combined with a steroid on six patients with severe COVID-19. It found that the treatment reduced both how long patients had the disease and how long they were hospitalized. A June case study published by some of the same authors had similar results for the patient it examined.
Given thalidomide’s history, however, researchers are understandably cautious about its repurposing. In a paper examining the evidence for thalidomide’s use against COVID-19, researchers at the American University of Beirut in Lebanon and Hamad Bin Khalifa University in Qatar noted that thalidomide is approved to treat very few conditions because of its serious side effects. These include causing blood clots and long-term nerve damage. “Repurposing thalidomide based on the first glance at its proven efficiency in some pulmonary inflammatory conditions is inadequate,” write the authors.
They also note that although there are two current Chinese clinical trials of the drug for COVID-19, neither has started recruiting participants yet, and both were set to be finished by June 2020. Although it’s unclear why this is, it might be because China has had very few cases of the disease since March. The trials are also small, phase two tests, with the larger having 100 patients and the smaller just 40. So despite its surprising promise, it’s unclear when, if ever, thalidomide might be used to treat COVID-19.
Melatonin
You might not think of melatonin as a drug at all; in the U.S, melatonin is considered a supplement and is not strictly regulated the way drugs are, although it’s a prescription drug in other counties. Melatonin is a hormone which helps regulate when we sleep and wake up, and many people take it to help them fall asleep. However, there’s conflicting data on whether it actually works as a sleep aid. In the U.S., melatonin is not approved to treat any medical condition, although it has been investigated, with mixed results, as a treatment for everything from cancer to high blood pressure.
So it would be surprising if melatonin were approved to treat any medical condition, let alone COVID-19. But many researchers think melatonin could benefit COVID-19 patients. A team of Chinese and U.S. researchers published a paper in June asserting that melatonin might be useful as a COVID-19 treatment because of effects it can have related to reducing inflammation, calming the immune system, and helping the body repair damage. Other researchers have echoed its promise, emphasizing that melatonin is very safe to use.
Research so far has been promising, but preliminary. A recent analysis done by researchers at the Cleveland Clinic found that patients taking melatonin were nearly 30 percent less likely to be diagnosed with COVID-19, and among African Americans, who have been particularly impacted by the pandemic, that number rose to 52 percent. Another study, which has not yet been reviewed by other scientists, found that both COVID-19 and other patients who had to use ventilators fared better when given melatonin.
“It is very important to note these findings do not suggest people should start to take melatonin without consulting their physician,” Feixiong Cheng, a computational biologist at the Cleveland Clinic’s Genomic Medicine Institute and the lead author on the first study, said in a press release. But he is “excited about the associations put forth in this study and the opportunity to further explore them.”
At least eight clinical trials are investigating if melatonin can be used either alone or with other treatments against COVID-19, including three in the U.S. The U.S trials range in size from just 30 participants to nearly 400, and other trials, like one in Spain and another in Mexico, were set to be completed already, although it’s unclear if they were or have yet yielded any results. The first U.S. trial isn’t set to finish until March 2021, so we may have to wait a while longer to know whether COVID-19 could become the first disease that melatonin is approved to treat in the U.S.
Although these treatments might not end up being as effective as newer, specially-developed drugs, repurposing older treatments, when done in a safe and careful way, can save money, time, effort, and even lives. Although none of these drugs are new, using them to successfully combat COVID-19 would give them new life, making them one piece of the puzzle that will eventually help end this global pandemic.